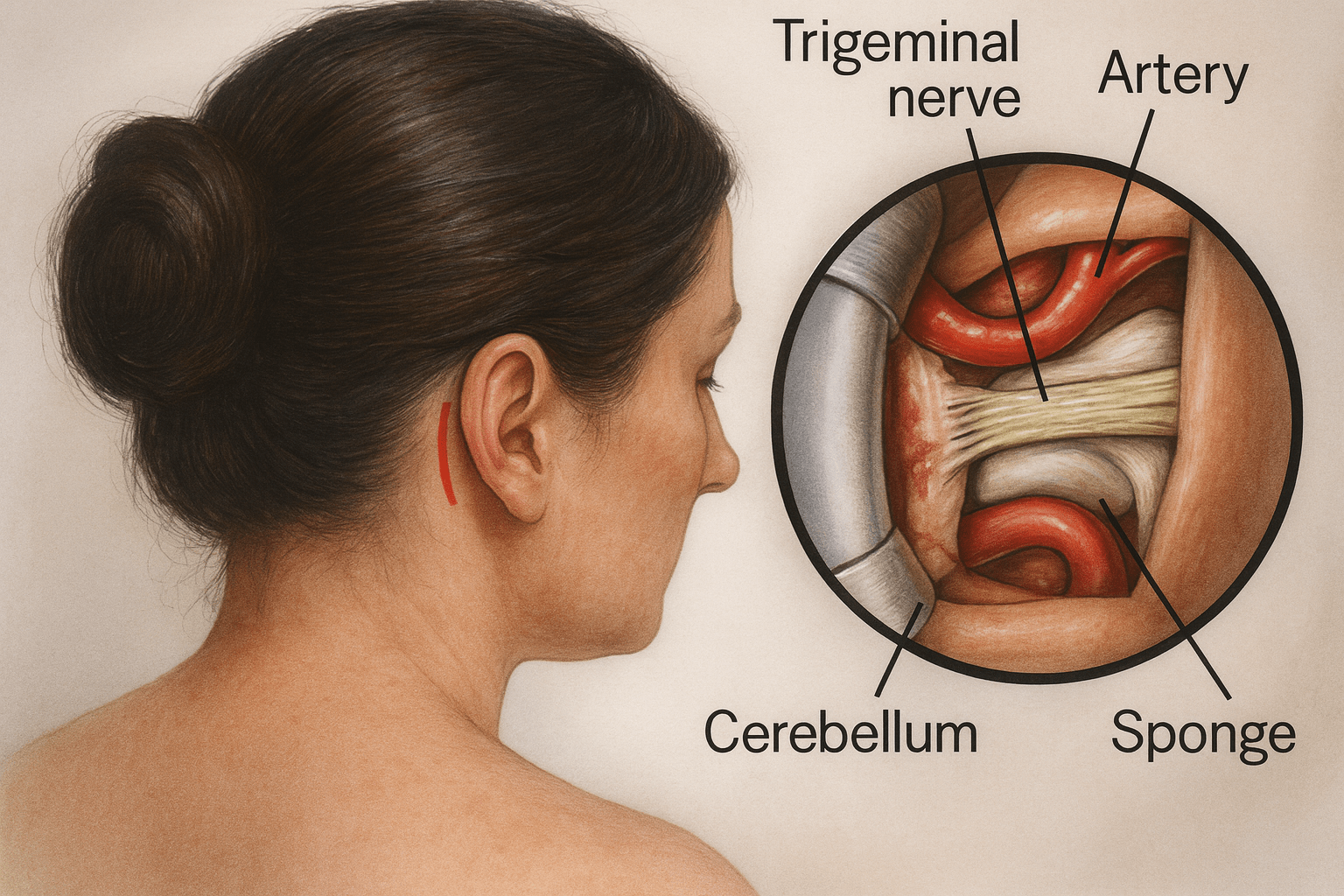
Goal of Microvascular Decompression (MVD)
Microvascular Decompression is widely-recognized as the “gold standard” treatment for trigeminal neuralgia, Eagle syndrome and hemifacial spasms, among others. It relieves pressure from a pulsating vessel that is pressing against a nerve, causing painful impulses from the face, ear or throat to either abate or stop altogether.
How Microvascular Decompression is Performed
Our neurosurgery clinic performs this procedure under general anesthesia.
The hair behind your ear is shaved, and a small part of your skull is then removed. Our expert neurosurgeons then identify the affected nerve, and pieces of Teflon are placed between the nerve and the offending blood vessel(s). The small area of bone removal is then covered with a thin metal mesh in order to complete this procedure.
Am I a Candidate?
You may be a candidate for MVD if you have:
- Trigeminal neuralgia that is not well controlled with medication
- Eagle syndrome
- Hemifacial spasm
- Facial pain isolated in the ophthalmic division
- Facial pain in all three trigeminal divisions
- Facial pain recurrence after a previous percutaneous or radiosurgery procedure
Because microvascular decopression treatment involves the use of general anesthesia and brain surgery, patients with other medical conditions or who are in poor health may not be candidates. MVD is not successful in treating facial pain caused by multiple sclerosis.
Because of the low risk of hearing loss, MVD may not be suitable for patients who have hearing loss in the other ear.
Schedule an e-consult here to learn more about your candidacy for MVD treatment at our South Florida neurosurgeon’s office.
Microvascular Decompression Treatment at The Morrison Clinic™
To help determine if MVD treatment is right for you, Dr. Morrison will ask you to consider:
- What are your symptoms and where are they located?
- When did you first develop these symptoms?
- Have your symptoms gotten worse over time?
- How often do you experience bouts of facial pain, and have you noticed if anything seems to trigger your facial pain?
- How long does an attack of facial pain typically last?
- How much are these symptoms affecting your quality of life?
- Have you ever had dental surgery or surgery on or near your face, such as sinus surgery?
- Have you had any facial trauma, such as an injury or accident that affected your face?
- Have you tried any treatments for your facial pain so far? Has anything helped?
- What side effects have you experienced from treatment?
Tests to Determine if MVD is Needed
Dr. Morrison will diagnose trigeminal neuralgia, as well as the other conditions MVD treats, mainly based on your description of the pain, including:
- Type: Pain related to trigeminal neuralgia is sudden, shock-like and brief
- Location: The parts of your face that are affected by pain will tell your doctor if the trigeminal nerve is involved
- Triggers: Trigeminal neuralgia-related pain usually is brought on by light stimulation of your cheeks, such as from eating, talking or even encountering a cool breeze
We may also conduct these tests to diagnose you, and determine any underlying causes:
- A neurological examination: Touching and examining parts of your face can help your doctor determine exactly where the pain is occurring and — if you appear to have trigeminal neuralgia — which branches of the trigeminal nerve may be affected. Reflex tests also can help your doctor determine if your symptoms are caused by a compressed nerve or another condition.
- Magnetic resonance imaging (MRI): Your doctor may order an MRI scan of your head to determine if multiple sclerosis or a tumor is causing trigeminal neuralgia. In some cases, your doctor may inject a dye into a blood vessel to view the arteries and veins and highlight blood flow (magnetic resonance angiogram).
Facial pain can be caused by many different conditions, so an accurate diagnosis is essential before proceeduing with MVD treatment.
Conditions that Microvascular Decompression Treats
MVD represents the “gold standard” first-line trigeminal neuralgia treatment; its aim is to free the nerve from any contact.
MVD surgery also is an effective treatment option for other siimlar conditions, such as:
- Eagle syndrome
- Hemifacial spasms
- Glossopharyngeal neuralgia
If you have any of these conditions, or their symptoms, and are ready to see if MVD surgery can help you re-gain your best quality of life, schedule an e-consult today.
MVD Aftercare and Positively Influencing Recovery
After surgery, you’ll be taken to the recovery room where vital signs are monitored as you awake from anesthesia. Next, you are transferred to the intensive care unit (ICU) for close observation overnight. You may experience some nausea and headache after surgery; medication can control these symptoms. When your condition stabilizes, you’ll be transferred to a regular room where you’ll increase your activity level (sitting in a chair, walking). In 1 to 2 days you’ll be released from the hospital and given discharge instructions.
Patients taking anticonvulsant or pain medication for trigeminal neuralgia prior to surgery will be weaned off the medications according to a schedule to decrease risk of withdrawal and side effects.
For your best quality of life, we recommend you follow the home care instructions from our South Florida neurosurgeon‘s clinic for 2 weeks after surgery or until your follow-up appointment. In general, you can expect:
–Incision care
You may shower the day after surgery and wash your hair with mild baby shampoo. Gently wash the incision area with soap and water every day. Don’t scrub or let the water beat hard on your incision. Pat dry.
If Dermabond skin glue covers your incision, don’t rub or pick at the glue.
Don’t submerge or soak the incision in a bath, pool or tub. Don’t apply lotion/ointment on the incision, including hair styling products.
You may hear strange noises (popping, crackling, ringing) inside your head. This is normal healing as air and fluid reabsorb.
Don’t color your hair for 6 weeks. If you cut your hair, use caution near the incision.
–Medications
Headaches are common after surgery. You may take acetaminophen (Tylenol).
Take pain medicines as directed by your surgeon. Reduce the amount and frequency as your pain subsides. If you don’t need the pain medicine, don’t take it.
Narcotics can cause constipation. Drink lots of water and eat high-fiber foods. Stool softeners and laxatives can help move the bowels. Colace, Senokot, Dulcolax and Miralax are over-the-counter options.
Anti-seizure medicine may be prescribed. Some patients develop side effects such as drowsiness, balance problems, or rashes. Call the office if any of these occur.
Our neurosurgeon clinic recommends that you do not consume anti-inflammatory pain relievers (Advil, Aleve), blood thinners, or supplements without approval.
–Activity
Get up and walk 5-10 minutes every 3-4 hours. Gradually increase walking as you are able.
Swelling and bruising of the ear or face may occur. It will take several weeks to go away.
Sleep with your head elevated and apply ice 3-4 times per day for 15-20 minutes to help reduce pain and swelling.