Morrison Clinic Uniquely Offers Discseel Procedure
South Florida Neurosurgeon
Home » Neurosurgery Treatments » Discseel Procedure
Goal of The Discseel® Procedure
The Discseel® Procedure is a minimally invasive spine procedure that allows patients to relieve their low back and neck pain without surgery, through the use of an FDA approved biologic fibrin sealant. This revolutionary treatment is now available at Morrison Clinic locations in both Manhattan, New York and Delray Beach, Florida, providing patients throughout the tri-state area and Southeast with access to cutting-edge spine care.
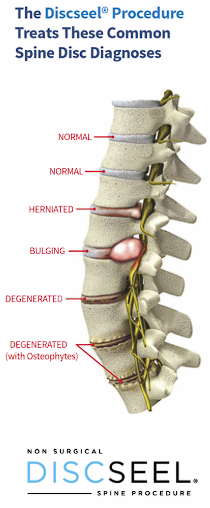
The Discseel® Procedure treats most spine pathology because it identifies and treats disc annular tears and fissures, which are the true and underlying cause of most spine issues including disc herniations, bulges, degeneration, and radiculopathy.
Even spinal stenosis and facet hypertrophy trace true origins to annular tears and fissures.
Contact Morrison Clinic for More Information, please call: (561) 485-4104
For NYC patients, please call: (917) 525-2981
How The Discseel Procedure is Performed
The Discseel® Procedure uses a substance called fibrin (which exists in human blood) that is an FDA-approved drug that is used off-label, analogous to corticosteroid used for epidural injections.
Corticosteroid is an FDA approved drug, but is not indicated for the epidural space, yet physicians recognize its help with patient’s back pain.
The Discseel® Procedure uses non-autologous fibrin in the same manner. A physician introduces it into damaged discs in the lumbar and/or cervical spine. It seals the disc, becoming a part of the disc, and then promotes the growth of disc tissue.
During the Discseel® Procedure, part of the process is to look for torn discs as evidenced through fluoroscopic guidance, called an annulogram, that provides x-ray images demonstrating disc tears within the annulus fibrous.
If the disc is shown to have a tear, fibrin is injected.
The goal of the fibrin is to seal torn, leaky discs and promote regrowth of disc tissue.
Treatments



Is this Treatment Covered by Insurance?
Discseel® is not currently covered by most insurance providers. Our NYC and Delray Beach locations offer flexible financing options and will verify your specific coverage.
Am I a Candidate?
- Any person with long lasting low back pain is a potential candidate.
- A person with low back pain who’s had surgery or a person with low back pain who prefers to avoid surgery is a potential candidate, because the cushion in the back known as the disc is the most common cause of low back pain.
Discseel® Procedure at Morrison Clinic™
- What are your symptoms and where are they located?
- When did you first develop these symptoms?
- Have your symptoms gotten worse over time?
- How often do you experience bouts of back pain, and have you noticed if anything seems to trigger your back pain?
- How long does an attack of back pain typically last?
- How much are these symptoms affecting your quality of life?
- Have you tried any treatments for your back pain so far? Has anything helped?
- What side effects have you experienced from treatment?
Conditions that Discseel® Treats
The Discseel® Procedure is used to treat patients with chronic low back pain and neck pain who desire to avoid surgery and who have failed to experience relief from surgery in the lumbar and cervical spine.
The focus is to provide the patient with a better quality of life, without surgery.
The Discseel® Procedure can treat conditions from bulging, herniated, degenerative disc disease to failed spine surgery such as a spinal fusion and artificial disc replacement; as well as treating low back pain, sciatic, and leg symptoms.

Discseel® Aftercare and Positively Influencing Recovery
If you are traveling from out of town, we recommend staying in a local hotel two nights following your procedure.
You will need to arrange for another driver to take you to your destination once you are discharged from the surgery center.
Discseel® often causes temporary increased discomfort because the ligaments surrounding your discs are stretched, and the procedure causes the beneficial extravasation (“flushing”) of inflammatory chemicals from your disc to your epidural space.
This is normal.
THINGS TO WATCH FOR FOLLOWING YOUR PROCEDURE:
- Fever (temperature above 101.5F/38.5C).
- New onset of incontinence.
- New onset of paralysis.
- Severe headache, allergic reaction, disorientation.
IF ANY OF THESE OCCUR, PLEASE CALL THE OFFICE. REPORT TO AN EMERGENCY DEPARTMENT OR CALL 911 IF YOU EXPERIENCE EXTREME NEW ONSET OF SYMPTOMS SUCH AS INCONTINENCE OF THE BOWEL AND/OR BLADDER OR RAPIDLY PROGRESSING WEAKNESS OF THE EXTREMITIES WITHIN A 24-HOUR PERIOD.
Following your procedure, your pain level may be high.
Accordingly, you will be offered prescriptions for pain medications and muscle relaxants which are to be used as needed.
You may also use over the counter anti-inflammatory medications, ice or a heating pad immediately following your procedure — ice is preferable.
It helps to “stay ahead” of your pain with medications, allowing you to be physically mobile, especially beginning the day after your procedure.
Many patients experience increased and/or changing symptoms in their lumbar spine or extremities varying from a few days to several months afterwards.
This is normal.
Use your pain medication prescribed by us and follow up with your local your doctor, if needed.
Patients are advised to restart their prior prescribed anticoagulant medication the evening of the procedure.
On the day of your procedure, do not operate a vehicle following your procedure or anytime while taking narcotics.
If you are traveling from out of town, we encourage you to stay in a local hotel two nights following your procedure, as well as have someone stay with you at your hotel overnight the first night just as a standard safety protocol per the recommendation of the American Academy of Anesthesiologists.
Activity
- Limit your activity during the first 24 hours following your procedure by relaxing in a reclining chair or bed but please get up the morning following your procedure and walk around your home or hotel.
- We prefer you NOT be on strict bed rest.
- You may use a pillow under your knees if you sleep on your back (if it helps with symptoms), or you may use a pillow between your knees if you are a side sleeper (if it helps with symptoms).
- This is not imperative, rather just a suggestion if it makes you feel more comfortable.
- To avoid disc re-injury, you should avoid improperly bending the spine, twisting of the spine or lifting heavy objects with your back.
- Avoiding these movements serves to avoid damaging your lumbar discs caused by compressive and shear forces on the discs.
- Proper body mechanics are vital to the longevity of the procedure, so we encourage you to avoid these movements as a lifestyle.
- Walking is a natural and gentle method of encouraging good circulation and creating the osmosis effect.
For NYC patients: Take advantage of Central Park, waterfront areas, and other walking-friendly locations for your recovery exercise.
- Osmosis keeps our discs healthy by moving nutrients around, thus allowing biologics the greatest opportunity to heal.
- Start walking a short distance the second or third day following your Discseel® procedure and gradually work up to a tolerable distance a few days a week over the next several months, letting pain be your guide.
- There is no specific guideline as it pertains to how many minutes to walk after the first few days following your procedure.
- Most patients begin a walking schedule each morning and evening after the first week following the procedure when the initial increase of post-op pain has passed.
- Listen to your body and use a commonsense approach. Follow the 10% guideline. When you feel ready to walk consistently, do it at a 10% level of what you did prior to your procedure.
- If you experience increased symptoms, cut back and do not walk as much until your body is ready. (More info below regarding the 10% guideline).
- When you begin feeling better and want to add activities you once enjoyed, please do so at 10% of what you used to do and let pain be your guide.
Please use commonsense approach with all activities, and most importantly, avoid spinal flexion and rotation as a lifestyle.
Many patients ask what the “typical recovery” is for patients following Discseel®.
The best way to communicate the recovery is to remember that lifelong habits likely contributed to your current condition, so make real life habit changes.
Avoid the two worst habits: flexing forward which damages discs by compressive forces, while rotation’s “shear force” tears disc’s annulus fibrosus.
Therefore, begin to lift and turn with your legs, lifting weights close to your center of gravity. No bending forward nor twisting. If you are an avid golf and/or tennis player, you’ll have to prioritize your life’s goals.
We recommend the “10% guideline”. Imagine what was typically 100% for you, and intentionally begin at only 10% of that activity until you feel comfortable.
When comfortable, which may be two days or two months, increase to 20% of your full activity, and continue increasing incrementally as you feel good. Walk and jog with soft shoes and avoid treadmills unless you’re sure to not lean forward on the handrail.
Contact Morrison Clinic for More Information, please call: (561) 485-4104
For NYC patients, please call: (917) 525-2981
Frequently Asked Questions
What type of exercise can I do after the procedure?
We would like patients to avoid bed rest except for the first night we want them to rest in a local hotel unless they live nearby and can rest at home.
We would like all patients to avoid flexion (bending over) and rotation (twisting) of the lumbar spine when possible.
We remind them that something got them into this position to begin with, which was likely a continuous motion of compressive (flexion) and shear (rotation) forces on the discs over time, so we encourage them to avoid activities that involve flexion and rotation.
When can I return to exercising?
You may begin walking a couple of days after the procedure. We do not want you on bed rest.
Discs get their nutrients through osmosis, so we encourage all patients to begin walking in small spurts usually on day 2-3 days after the procedure. For the first 4-6 weeks, we encourage walking daily.
After the first 4-6 weeks, depending on the patient’s symptoms, they may add other activities into their exercise regime but only at a 10% level and see how they feel afterward.
Based on how they feel at a 10% level, hold there for a few weeks, and slowly add to it as they feel better. Use a common-sense approach.
Can I still use my inversion table?
While we do not tell a patient “no”, we have found more patients seem to injure themselves by getting on and off an inversion table from improper body movement, so we say, “Use at your own risk but recognize many patients re-injure themselves getting on and off of them.”
Can I have a massage right after the procedure?
Yes, you may have a massage one-week post procedure. You may want to avoid a deep tissue massage the first couple of weeks, but a normal massage is okay.
Make sure your massage therapist does not stretch you.
When may I return to seeing my chiropractor?
You may go back to your chiropractor for follow up care shortly after the procedure so long as they do not manipulate your spine in any way.
Please avoid all “popping” and manipulating of your spine.
Manipulating the spine may result in tearing a disc if the chiropractor places shear forces on the discs.
We like chiropractors and think they are great for offering post-operative care (same with a physical therapist), so please if you consider going back to their care, do so at your own discretion but please ask them to avoid ALL shear and compressive forces on the lumbar and cervical spine.
How long will I be off work?
Most patients return to work after about 3-5 days. However, if you need more time off, speak to your physician to see if they can write a letter on your behalf to allow you additional time off from work.
We strongly advise patients to avoid any heavy lifting for 4-6 weeks.
How long after the procedure can I go home?
Patients are free to leave if accompanied by someone after they leave the post-op area.
We strongly advise that the patient does NOT drive himself or herself home.
Most patients are in post-op for about 30 to 60 min.
Will my discs plump back up to their original youthful size?
While some patients’ discs immediately plump back up, our goal is not to plump up the discs, but rather, our goal is to promote regeneration of spine tissue where tears reside, thus stopping the disc that have inflamed the spinal nerves and nociceptors (nerves that lives within the outer portion of the disc) from leaking.
How long does it take for the patient to begin feeling relief?
Based on our research the majority of our patients “turn the corner” in 3-6 months.
However, many patients feel better several weeks following the procedure, and a minority of patients as late as 8-12 months.
So, it’s important to recognize based on past research that we won’t know the full outcome of the patient’s procedure until one year out so set the expectations that we do not expect them to “turn the corner for many months.”
Do you have a Manhattan office location?
Yes, Morrison Clinic now offers Discseel® procedures at our Manhattan location, making this revolutionary treatment accessible to patients throughout New York City and the tri-state area.